Diclazuril 8.3% / Levamisole 3% / Vitamin E 656 iu Paste For Treatment of EPM in Horses

Equine protozoal myeloencephalitis (EPM) is a disease of the horse that affects the central nervous system. Equine obviously refers to the horse, protozoal refers to the type of organism that causes the disease and myeloencephalitis refers to that portion of the animal, which is damaged. “Myelo” refers to the spinal cord and “encephalitis” refers to an infection/inflammation of the brain.1
Thus, EPM is a disease of the brain and/or spinal cord of the horse caused by a protozoan organism.
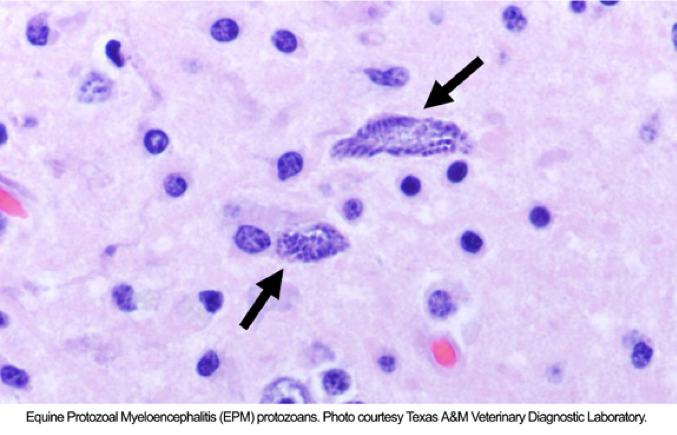
Protozoa are single-celled organisms, and are the smallest and most simplistic members of the animal kingdom. The name given to the protozoan organism shown to be the primary causative agent for EPM is Sarcocystis neurona.
Background
Equine protozoal myeloencephalitis was described in the 1960s as "segmental myelitis." By 1974, it was determined that this disease was caused by a protozoan organism. In 1976 it was concluded that some type of Sarcocystis organism was the culprit. This organism (Sarcocystis neurona) was first isolated from the spinal cord of a horse with clinical signs of EPM in the early 1990s. In the late 1990s, another organism called Neospora hughesi was shown to also cause EPM in horses,1 but in rare instances only. EPM is a disease primarily of the Western Hemisphere and is not commonly seen in other parts of the world.
According to MacKay and Morgan, many horses are exposed to the S. neurona parasite, evidenced by specific testing that has been on blood samples taken from horses around the country. Blood samples are evaluated to determine if it contains antibodies specific to the S. neurona organism. If the sample contains these antibodies, then we know the horse has been exposed to this parasite and has mounted an immune response, or is seropositive with antibodies against S. neurona. This does not, however, reveal whether or not the horse has or will ever develop EPM. Fortunately, only a very small percentage of horses seropositive to either parasite (S. neurona or N. hughesi) ever develop the disease we call EPM.
How Do Horses Develop EPM?
Although much has been learned in recent years with respect to the life cycle of S. neurona, there remains much that is unknown. Sarcocystis neurona has a complex, two-host life cycle. This life cycle includes both a definitive host and several possible intermediate hosts. For clarification, the definitive host is that animal which sheds in its feces an infective form of the parasite, S. neurona.1 The intermediate host is that animal which does not shed an infective form but is a host where the parasite resides and is necessary for the parasite to complete its life cycle.
In 1995, the opossum was determined to be the definitive host of this parasite (there may possibly be other definitive hosts for this organism and we have just not yet identified them). The opossum sheds the infective form of the parasite in the feces; we call this infective form a “sporocyst.” The sporocyst is then ingested (eaten) by the horse. Once inside the horse, there is much that we do not know regarding what occurs next. The parasite does go through a maturation or reproductive phase and eventually produces a form of the parasite we call “merozoites.” Eventually (in only a very small percentage of horses) the merozoites reach the central nervous system, damage this vital area and create the disease condition we call EPM.1
Several animals fall into the category of intermediate hosts for S. neurona. Among these are skunks, armadillos, raccoons, cats and sea otters. Since it is not believed that the horse is a natural host for this parasite, the horse is often referenced as an "aberrant intermediate host."2
Since a great many horses in the Western Hemisphere are seropositive for EPM but never develop the disease, it is likely that horses that do develop EPM do so because they are, or become, immunocompromised.
Symptoms and Diagnosis
Since EPM is a disease of the central nervous system (brain and spinal cord) and can affect multiple locations within the brain and spinal cord, the signs and severity of this disease can vary dramatically.
In recognizing and referencing symptoms of EPM, veterinarians usually cite "The 3 A's” of this disease: Asymmetry, Ataxia and Atrophy.
1. Asymmetry is a term we use to describe a symptom that is worse on one side of the body than on the opposite side. In other words, with EPM, the signs are generally worse on the left side than on the right or visa versa.
2. Ataxia is a term we use to describe incoordination or the inability of the horse to know exactly where its legs are, resulting in inability to move its legs and trunk normally.
3. Atrophy describes a condition where the muscles shrink from their normal size. With EPM, this results from damage to the nerves that normally control or “innervate” these muscles. Muscle atrophy is not seen in all cases of EPM, so it is not as consistent a sign of disease as is the asymmetrical ataxia.1
Thus, when EPM is present, "we will see horses that are uncoordinated and this uncoordination is usually worse on one side of the body as compared to the other side. These horses may or may not develop muscle atrophy. It is also common to see muscle weakness in these horses."1 Some horses may display abnormal gaits, lameness and loss of sensation along the face, neck or body. Paralysis of the muscles of the eyes, face or mouth may occur and this will be evident by drooping eyes, ears or lips. Horses may also demonstrate a head tilt, poor balance and difficulty in swallowing or vocalizing. On rare occasion, even seizures and collapse may occur.
EPM may progress rapidly or very slowly. Horses generally deteriorate over time, but some plateau for a period of time, only to worsen days, weeks or even months later. Strangely, it is reported that most horses afflicted with this debilitating disease continue to have a bright, alert temperament.
Unfortunately, there is no single test for EPM that can be done which is 100% accurate in the live horse, although there are tests that can be utilized by the veterinarian to support their diagnosis of EPM, as well as to rule out other diseases which may present like EPM.
The most important evaluation done by the veterinarian in cases of suspected EPM is a neurologic examination.2 This is a specialized exam that is done to evaluate the function of the central nervous system of the horse. It may also be necessary that radiographs be taken of the neck region of the horse to determine if there is compression on the spinal cord, since clinical signs from pressure on the spinal cord can look very much like EPM.
The veterinarian may also draw blood during the examination process. In some cases, he or she may decide to collect spinal fluid from the horse by doing a spinal tap. The most accurate of the currently available EPM tests require submission of both blood and spinal fluid to the diagnostic lab. Analyses of blood and spinal fluid samples both support the diagnosis of EPM and also help rule out other diseases of the central nervous system.1
Prevention and Treatment of EPM in Horses
Treatment of EPM is challenging because S. neurona is an intracellular parasite and an expert in avoiding immune system attack. The three different anti-protozoal treatment modalities that have been typically used work on entirely different pharmacological principles. Traditionally, EPM was treated with combinations of pyrimethamine and a sulfonamide.2 This combination was, for many years, the only known treatment for EPM, although the duration of treatment was often prolonged.
In recent years however, medications to treat EPM have been refined significantly by custom compounding pharmacies. As indicated above, veterinarians did use the combination of sulfadiazine and pyrimethamine in the early days of EPM treatment, and it previously could be obtained as a compounded drug.
More recently, formulations containing diclazuril have been approved by the FDA. The function of diclazuril is in attacking the chloroplast function of the protozoa. These novel formulations often include antiparasitics such as levamisole, and Vitamin E to provide support for muscles that have atrophied.
For the prevention and treatment of EPM, the formulations mentioned above are available through custom compounding pharmacies in paste or suspension form.
Paste Preparations - Pros & Cons:
Pros
- Easy dosing accuracy
- Less loss of medication due thicker consistency
- Less loss of medication due to spills
Cons
- Can amount to a lot of tubes to prepare/transport per treatment (30ml per day = ½ of 60ml tube) (15 tubes = 30 day treatment)
- Possibility of loss of tube(s)
- Difficult to travel with multiple horses on treatment
- Can be thick
Both the paste and suspension versions are given orally, but the type chosen will usually be contingent upon the owner or veterinarian's personal preference, the animal's temperament, the number of animals that need to be treated, travel considerations, and the like.
1MacKay, R., Morgan, K. DVM. Equine Protozoal Myeloencephalitis. aaep.org.
2Equine Disease Quarterly, Jan. 2007.
About NexGen Pharmaceuticals
NexGen Pharmaceuticals is an industry-leading veterinary compounding pharmacy, offering sterile and non-sterile compounding services nationwide. Unlike other veterinary compounding pharmacies, NexGen focuses on drugs that are difficult to find or are no longer available due to manufacturer discontinuance or have yet to be offered commercially for veterinary applications, but which still serve a critical need for our customers. We also specialize in wildlife pharmaceuticals, including sedatives and their antagonists, offering many unique options to serve a wide array of zoo animal and wildlife immobilization and anesthesia requirements.
Our pharmacists are also encouraged to develop strong working relationships with our veterinarians in order to better care for veterinary patients. Such relationships foster an ever-increasing knowledge base upon which pharmacists and veterinarians can draw, making both significantly more effective in their professional roles.
Disclaimer
The information contained in this blog post is general in nature and is intended for use as an informational aid. It does not cover all possible uses, actions, precautions, side effects, or interactions of the medications shown, nor is the information intended as medical advice or diagnosis for individual health problems or for making an evaluation as to the risks and benefits of using a particular medication. You should consult your veterinarian about diagnosis and treatment of any health problems. Information and statements have not been evaluated by the Food and Drug Administration ("FDA"), nor has the FDA approved the medications to diagnose, cure or prevent disease. Medications compounded by NexGen Pharmaceuticals are prepared at the direction of a veterinarian. NexGen Pharmaceuticals compounded veterinary preparations are not intended for use in food and food-producing animals.
NexGen Pharmaceuticals, LLC does not recommend, endorse or make any representation about the efficacy, appropriateness or suitability of any specific dosing, products, procedures, treatments, services, opinions, veterinary care providers or other information that may be contained in this blog post. NEXGEN PHARMACEUTICALS, LLC IS NOT RESPONSIBLE NOR LIABLE FOR ANY ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER INFORMATION, SERVICES OR PRODUCTS THAT YOU OBTAIN THROUGH THIS BLOG POST.



